Cream and Crisps
(41) The opposite of old people are new-borns. For a long time, my greatest fear in emergency service was that of being called to a delivery. The gynaecologists have adapted this „planned emergency“ so thoroughly that other physicians are largely lost in this field, due to our lack of experience. In due course, I did get some of that, too. In emergency services, deliveries are mostly completed already when the doctor finally arrives, or it has not come so far yet. The biggest danger is probably associated with stopping an advanced delivery with drugs (if very advanced, even drugs cannot do that). The closed I have been to that experience occurred just in front of our hospital when I arrived after a mission late one evening. A screaming, pregnant woman was supported by some people who tried to comfort her. I followed the call and got the impression that the delivery was taking place already, so we brought her a few meters further into the doorman's small office and placed her on the floor. I shall never forget the face of the doorman on call as I tore down her trousers and soon after drew a baby out, as the magician does with the rabbit of his high hat. I asked him to require enforcement from the maternity department, but he was unable to be of any use for some time afterwards. The baby survived the unusual delivery without any problems.
(42) When talking about fear, I come to think of the only mission I had to the victim of a poisonous snake. This was clear from the beginning, so I asked if the snake was still creeping around. As they answered from the Central that it was back in its terrarium, I declared that I would also come. Since it is an exotically animal and the patient with his leg stasis was at first well off, the doctor who had required me and I talked with a specialist at the Tropemedical Department in Basle, who suggested that the patient and the anti-poison would meet each other in Lörrach. We returned there without signal, and in the meantime I got the patient's permission to make some fun at the intensive care unit. I took some rubber rings from the ambulance and put in a plastic bag, at first keeping it hidden at the bag upon admittance. Having explained what I knew about, I suddenly brought forward the bag while saying, „and would you believe that all this trouble could arise from such a small snake?“ The two nurses present rescued themselves by escape to the adjacent department while the doctor I had talked to increased his distance of safety considerably. A few hours later, there was nothing to joke about, but the patient managed also this critical phase and was discharged three days later.
(43) „I have no time to be ill now,“ is sometimes heard. Accidents and diseases never comes while planned or even suitable. For the severely injured it may be like the end of the World. To me, it was sometimes necessary to see other aspect to which the involved persons could, understandably, not understand as funny. Such appeared with the collision of a bicycle and an air plane (a small one, after all), which happened at a local aerodrome when a one motored plane was about to start and a man crossed the lawn. The pilot almost succeeded to stop the plane (or there had been nothing for me to do there), which now was placed vertically with the tail pointing upwards. Beside it, a twisted bicycle bore witness that the collision was not completely avoided while a seriously wounded man let assume that it was possible to survive a collision with an air plane. I arrived with the helicopter and was later occupied for six hours with the operation - not al all funny.
(44) Another man survived colliding with a train on bicycle, unfortunately with permanent paraplegia. I arrived by car but required the helicopter to fly the patient to Freiburg where I explained about the accident. Responding the stupid question, which involved patient was present here (anaesthetized and intubated), I answered: „This is the engine driver - you should have seen the cyclist ...“
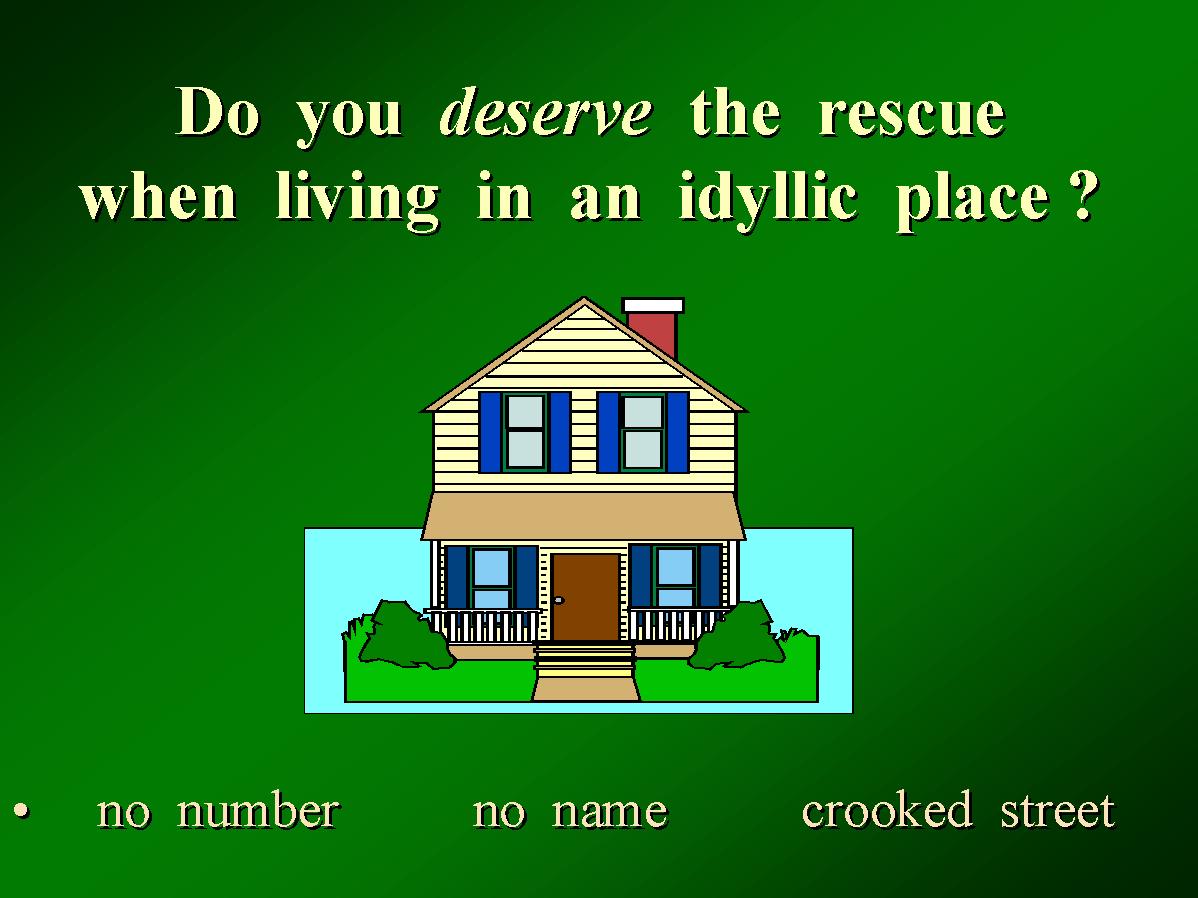
In Germany, I started at the anaesthesia department of the County Hospital of Eutin, situated in the North between Lübeck and Kiel. The rescue service was a secondary job, but the anaesthesia department was taking care of missions with a rather big Bell helicopter plus a much less utilized ground rescue service (same doctor!). We had many missions but not so many which were particularily necessary. On the other hand, many cases were known where our presence would have been desirable but where we were not asked to come. It remains strange to me that the Europeans (not just the Germans) have not worked for an improvement of this economical mismatch - on the contrary, the emergency physician is increasingly used = for less serious conditions, the central does not care to find out where the doctor could really be of any use but releases the alarm according to a catalogue. Once there, the emergency physician is held up by useless diagnostic measures and time-consuming bureaucracy (increasingly large mission protocols).
Because air rescue has been known in Germany since 1970, it could be expected that helicopter landing places (helipads) would be particularly sophistically. On the contrary, the regional hospital had generally much better landing facilities than the university hospitals, due to various human weak points which shall not be commented further here. If we were going to deliver patients to the University Hospital Eppendorf in Hamburg, it was necessary to interrupt the game at a near football place, an event which occurred rather often. We landed and were with the patient transferred to an ambulance, with which we drove to the young specialists who knew everything better and asked why this and why not that - I believe it has always been so in the university departments. After having received an impressive rebuke, we drived back to the helicopter, where the pilots were always not present. They were gone to visit Aunt Frieda. Later, they came back with a full mouth, cream and crumbs around, and we could fly back to Eutin or fuel in Hamburg’s „Fuhlsbüttel“ airport. Having experienced this a couple of times, I started to get curious about this Aunt Frieda. Finally, I was joined by another doctor. The patient was well off, so I decided to send him off to learn from the young stars in Eppendorf as a part of his education while I joined the pilots.
Fig. 14: Aunt Frida’s coffee table.

(45) I think that our pilots had a good time. In Eutin, they were placed for our disposition by the border gendarmes (Bundesgrenzschutz), which in this way had a useful training of their men. While the doctor and paramedics were taking care of a patient with a spinal trauma after a fall from a cherry tree, the pilots took care about the remaining cherries. By the way, it was almost always cherries, seldom other fruits, and having seen their branches break in the most unbelievable fashions, I have decided to buy our cherries at the local market and leave ours in the garden to the birds. One of my colleagues gave up resuscitation - perhaps good so, there was no room for any patient, the helicopter was full of flowers (one of the pilots were getting married).
When I started to work in Lörrach, the helicopter turned out to be much smaller (at first BELL 105S, now Agosta). It belongs to the Swiss Air Rescue (REGA) and is, to increase the confusion, based in the airport of Basle-Mulhouse („Euroairport“) on French ground. Until 1987, we were in charge of most of the mission, later the Department of Anaesthesia, Kantonspital Basel took over the vast part of airborne missions. The co-operation between Lörrach and Basle over the border is much better than the co-operation between two cantons in Switzerland. We registered no strive within the co-operation with French authorities - there was no co-operation at all. Fortunately, I was only upon rare occasions active on French ground.

My last mission as emergency physician in 1997 was a good occasion to stop: a successful resuscitation of a middle age man. Of course, I have also abused the possibility to avoid mentioning missions where I did not make a very brilliant figure. For that part, it is possible to read some of them among the case-reports (also including the new wisdom gained by colleagues) in my book about a professional, physician-supported rescue service – the idea is the we should not necessarily all make the same mistakes for learning from them.
In conclusion,
I must say that it was an interesting job. At the emergency
site, there were few problems that could not be dealt with – if you know
what to do, what may help or at least not deteriorate matters, there is
no reason to despair from the task, and it is often a most positive experience
being able to offer something that others may not be able to do. Ability
of improvisation is a necessary requirement, but stereotypically appearing
emergencies call for a standardized attitude. And exactly while I believe
to have found an answer to many problems, I have suffered many frustrations
from the lacking interest, both regionally and internationally. It has
not been qualitatively better that interest has quantitatively improved
– on the contrary, it is now even more difficult to favour any solution
which is not accepted by the majority. And it is as if this prostitution
for old-fashioned and simple solutions, which are generally found in medicine,
is even worse in emergency medicine.
As a result, I enjoy the experience which has passed
but I do not miss it. Many others have taken my place, there is no vacuum
left and after 17 years at the „front,“ a more quiet occupation can be
preferred without getting a bad conscience.
Best
Intentions - the previous chapters:
In the shadows of deathPrehospital Emergency Medicine, 2nd EditionNew methods incidental appearence
Novel techniques vs. old standard
Frustrations with fire
Dyspnoea
Problems are arising
Revised May 15, 2001